Intertrochanteric fractures are a common orthopedic injury that imposes significant morbidity on patients and costs to the healthcare system. Surgical fixation is the main method of treatment. Surgery within 48 hours of injury reduces mortality. Despite advances in implant design and minimally invasive techniques, failure rates remain as high as 9% to 16%. Although the risk of failure is multifactorial, optimizing surgeon-related factors is critical.
Optimizing trochanteric fracture fixation requires several key steps:
1. Preoperative Planning
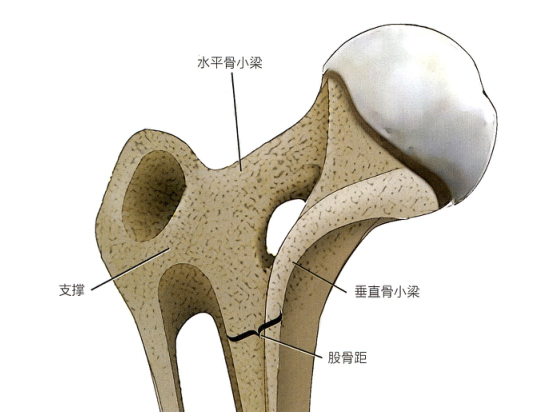
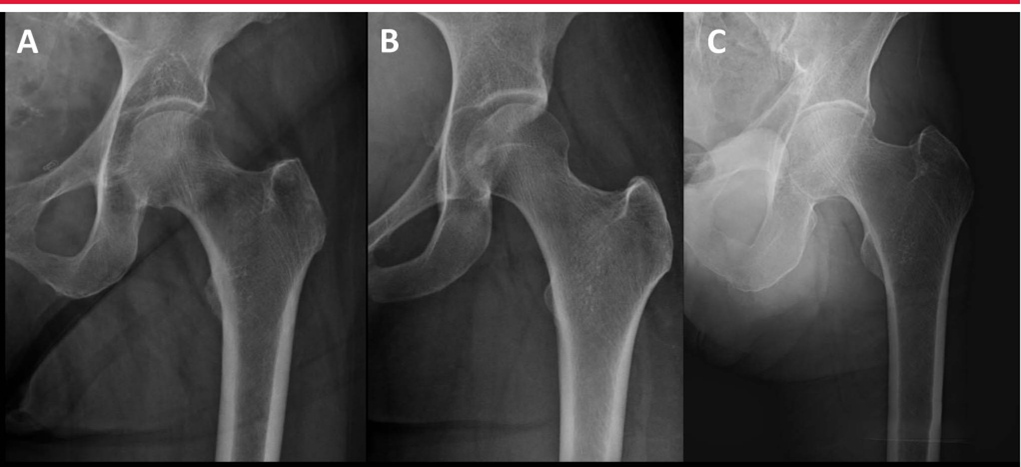
Specialized hip x-rays are necessary to evaluate fracture morphology. Although the relationship between the tip of the greater trochanter and the center of the femoral head is usually coplanar, anteroposterior pelvic or contralateral hip radiographs can help evaluate native anatomy and potential coxa valga or coxa varum. (coxa vara) (A normal neck-shaft angle in the picture below, B coxa valgus, C coxa varus)
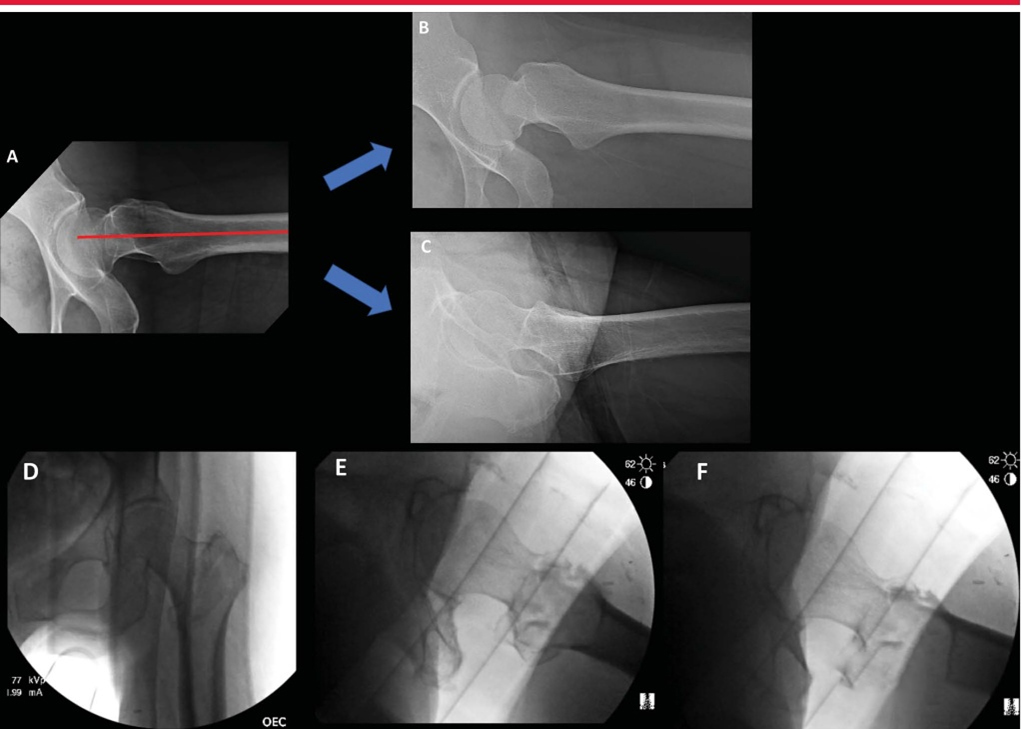
Internal rotation traction radiographs are particularly useful in preoperative planning. Khurana et al demonstrated that internal rotation traction radiographs significantly improved diagnostic accuracy, reliability, and interobserver agreement in proximal femur fracture classification. Additionally, preoperative traction radiographs can help the surgeon determine when closed reduction maneuvers are likely to be successful (Figure 2).
2.Determine the type of injury in troublesome intertrochanteric fractures
The optimal treatment of “unstable” intertrochanteric femoral fractures remains controversial. Recent literature suggests that A2 fractures of AO/OTA due to significant posteromedial comminution can be treated with extramedullary or intramedullary devices, but the success rate is uncertain. In contrast, type A3 fractures with lateral wall extension require intramedullary fixation. Several studies have shown that an intact lateral wall is required for successful treatment of intertrochanteric fractures with extramedullary implants. Hsu et al demonstrated that lateral wall thickness less than 20.5 mm is a reliable predictor of postoperative lateral wall fracture. The latest 14th edition of Campbell’s Orthopedic Surgery also clearly states: For unstable intertrochanteric fractures (A3 fractures and some A2 fractures), the best treatment is to use intramedullary nail fixation. (p2635)
Note: Diagram of lateral wall thickness. On the X-ray anteroposterior film, 3cm below the innominate nodule of the greater trochanter is used as a reference point, and then a straight line is drawn at an angle of 135° with the femoral shaft. The distance from the reference point to the fracture line is the lateral wall thickness (in millimeters)
Reversed intercarceral fractures present special challenges with reduction and implantation. A distinction needs to be made between high-energy and low-energy trochanteric fractures because these fractures “appear” differently (image below). While low-energy fractures can be successfully treated with closed reduction on the fracture operating table, high-energy fractures often require percutaneous or open reduction techniques.
Lateral fluoroscopic view of the left hip shows considerable displacement of the fracture fragments despite adequate traction and rotation on the fracture operating table.
3.Choose The Right Implant
Treatment of hip trochanteric fractures has evolved with changes in implant design. Sidewall integrity is the most important determinant of implant selection. Although subtrochanteric fractures are most commonly treated with long intramedullary implants, blade plates and proximal femoral locking plates may also be used. The indications for short versus long nails in the treatment of intertrochanteric fractures are controversial, and recent studies have shown that fracture rates are comparable between the two implants, while short nails have the benefits of shorter operative time and reduced blood loss. The short nail avoids the potential femoral arch and cortical perforation mismatch of the long nail. Fracture morphology is an important factor to consider when selecting nail length. Long nails may be more suitable for treating reverse intertrochanteric and subtrochanteric fractures.
The use of helical blades or screws to stabilize the cranial spine remains another topic of debate in implant design. Proponents of the helical blade emphasize its ability to prevent rotational deformity while reducing bone loss, while proponents of screw implantation argue for its increased biomechanical strength. The authors’ preferred method is cephalomedullary fixation using lag screws.
4. Obtain And Evaluate Appropriate Fluoroscopic Imaging
Intraoperative fluoroscopy is commonly used to evaluate fracture reduction and fixation. In order to evaluate fluoroscopic views during fracture fixation, one must understand the proximal femoral relationships of the intact femur and how they vary with fluoroscopic beam position, leg position, and normal anatomical variations. Images of the proximal femur show the standard relationship between the tip of the trochanter and the center of the femoral head. When the proximal femur is rotated externally, the angle of the femoral neck axis increases and the femoral neck appears to shorten (image below).

X-ray shows the AP fluoroscopic image of the same hip from internal rotation (IR) to external rotation (ER). Note the change in femoral contour of the hip from IR to ER. Note the appearance of the neck-shaft angle as it changes from flexion/IR to flexion/external rotation. Likewise, hip flexion and extension can significantly change the perspective of cervical axis angle. In the study by Bhashyam et al., hip flexion, extension, and rotation had a synergistic effect on the measurement of NSA. When the hip flexion and extension were within 10° of the neutral position, the measurement error was minimal. Because the affected hip joint tends to flex and internally rotate, this can give the illusion of increased varus.
Intraoperative lateral hip fluoroscopy for evaluation of reduction and implant. A, Lateral image best suited to the implant showing collinearity of the femoral head, femoral neck, and femoral axis. B, Lateral radiograph of the same hip joint in internal rotation. C, Externally rotated lateral image of the same hip, optimal for evaluation of anteromedial cortical support and reduction of trochanteric fractures. D – F, Intraoperative fluoroscopic images obtained in the supine position on the fracture table showing AP (D), lateral implant (E), and lateral reduction (F) views.
5. Perform Safe Open or Percutaneous Approaches
To achieve a perfect lateral position, the C-arm can be placed in a flat, horizontal position and then rotated (“rainbow up”) approximately 15° to match the patient’s natural anteversion and align the femoral head and neck (image below) ).
Although most low-energy peritrochanteric fractures can be treated with closed reduction, for some high-energy injuries, an open Watson-Jones or subfemoral approach can be used. The Watson-Jones method is commonly used to treat intertrochanteric and peritrochanteric fractures at the base of the neck.
6. Obtain and Maintain Fracture Reduction
The affected limb is usually placed in the supine position on the fracture operating table, traction and internal rotation of 15° are performed to achieve reduction. It is helpful to use the contralateral uninjured limb as a control, with the patella centered and the ipsilateral proximal femur fluoroscopic view as a reference. Critical assessment of radiographic reduction requires assessment of the anteromedial cortical support. Because the femoral calcar is frequently disrupted and comminuted in peritrochanteric fractures, the anteromedial cortical buttress provides the final structural restraint to telescopic fracture fragments. On the AP view, anatomical or positive anteromedial cortical support reduces controlled collapse of the fracture.
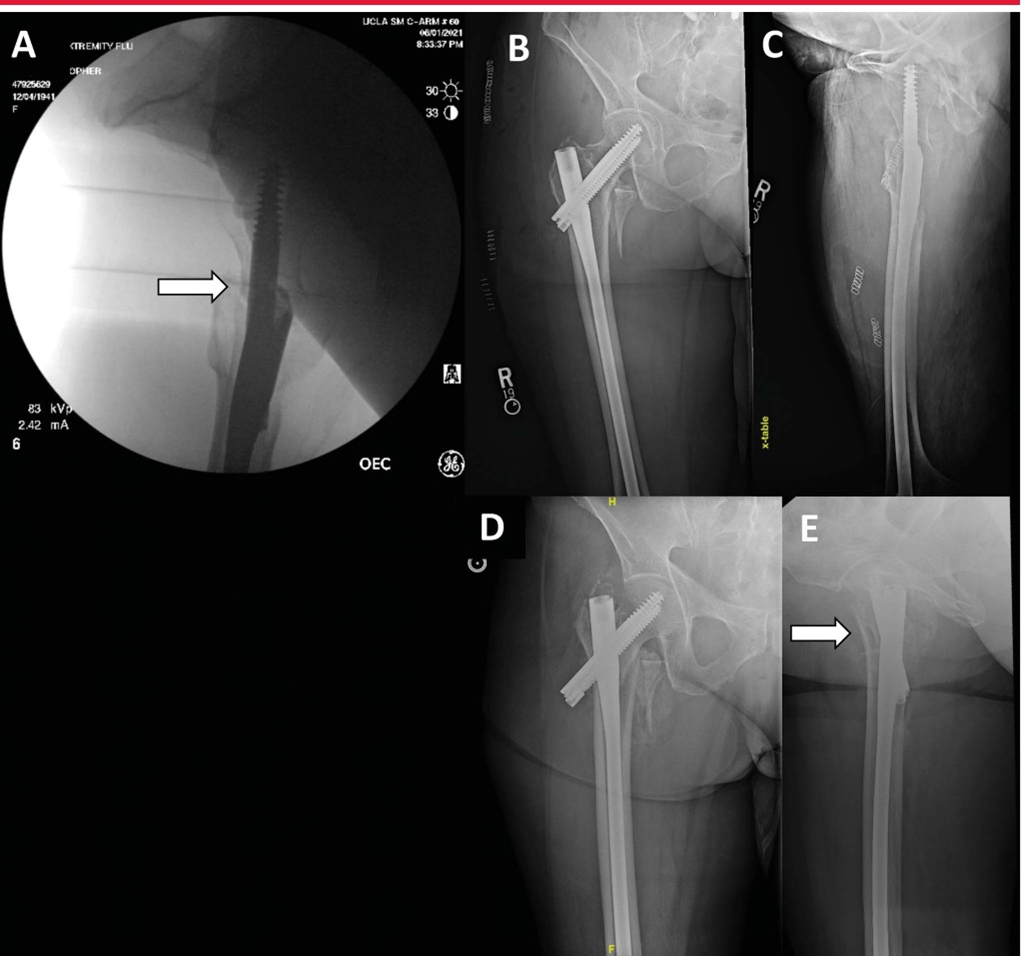
Lateral reduction view shows anteromedial cortical support (arrow). B, Postoperative AP image showing cortical alignment. C, Postoperative lateral image shows deformation of the anteromedial cortical support. D-E, AP and lateral views show significant collapse (arrow) 6 weeks after surgery.
Lateral anatomic reduction may be difficult, possibly because of the strong limitations of the iliofemoral ligament. It prevents anterior displacement of the femoral neck. The technique that can be used is to place Schanz pins from anterior to posterior along the medial and lower neck. This allows the anteromedial cortical support to be elevated to anatomic reduction and/or positive reduction.
7. Use Auxiliary Reset Tools When Necessary
A variety of assistive techniques and tools are available for fracture reduction, including pointed reduction forceps, cerclage wires, bone hooks, ball pin pushers, collinear forceps, and unicortical plates (image below).
A and B, Injured AP and lateral x-rays of the right hip showing comminuted fracture of the hip trochanter. C, Fluoroscopic image showing multi-point reduction clamps and cerclage wires used for reduction. D, AP pelvis shows good reduction of peritrochanteric fracture after surgery. E, AP postoperative image shows good fracture reduction and reconstruction nail placement. F, Lateral image shows a well-positioned and well-reduced peritrochanteric hip fracture. G, Shown are auxiliary percutaneous reduction tools, including (from R to L) Cobb, bone hook, collinear forceps, and ball peg pusher.
8. Carry Out Correct Implant Placement
Optimal internal fixation position is critical to maintain fracture reduction and reduce the risk of internal fixation failure. Openings, in particular, can significantly affect overall coronal and sagittal alignment of fractures. Intramedullary devices for treatment of peritrochanteric fractures can result in malreduction of the implant. The preferred approach is to align the long axis of the implant with the femoral axis to avoid varus malreduction, which is usually medial to the trochanteric tip. To align with the femoral canal in the sagittal plane, the starting point should be approximately 5 mm posterior to the apex of the trochanter to allow for its anterior offset. For subtrochanteric fractures, it is especially important not to start the sagittal plane too anteriorly. Biomechanical and clinical studies generally agree that the appropriate position of the screw or spiral blade should be in the middle of the lateral position, the middle or lower position of the AP position.
A, X-ray shows a 74-year-old woman with a left intertrochanteric fracture of the hip. B, Lateral image shows a comminuted intertrochanteric fracture of the femur. C, Postoperative AP image shows valgus reduction and inappropriate tip-to-tip distance. D, Postoperative lateral image shows larger end-to-end distance. E, AP image 6 weeks after surgery shows varus collapse and spiral blade incision. F, Lateral image 6 weeks postoperatively shows the spiral blade incision.
Disclaimer: This article comes from professional journals and books and is edited by Orthopedic Garden. If you have any copyright issues, please contact us.
Post time: Dec-08-2023